A migraine is more than just a bad headache. Learn more about what causes migraines, the symptoms, and how to cope when you’re experiencing an attack.
When your head is pounding, the first thing you probably ask yourself is: Could this be a migraine? “It’s very common for people to think that a migraine is a tension, sinus, or allergy headache. A lot of people are either undiagnosed or misdiagnosed,” says Bradley Katz, MD, a neuro-ophthalmologist at the University of Utah’s Moran Eye Center who specializes in treating migraine-related light sensitivity.
Migraines affect more than 36 million people in the United States, and those who are at higher risk include women, those in their 30s and 40s, and those with a family history. Migraines can be episodic (you get them sporadically) or chronic (you get them 15 or more days a month for more than three months).
Wade Cooper, DO, director of the University of Michigan’s Headache and Neuropathic Pain Clinic in Ann Arbor, thinks of a migraine as a neurologic reflex. “During a migraine, the lining of the brain gets an inflammatory signal that irritates the pain nerves, and those send the signal deep into the brain. Then the brain activates a cascade of hypersensitivity to lights, sounds, and smells,” he says. “Anything that irritates the nervous system can activate that reflex.”
The following info can help you figure out what might be going on in your head. “The sooner you find out if you are having migraines, the sooner and better they can be treated before their frequency increases,” says Santiago Mazuera Mejia, MD, a neurologist at the Sandra and Malcolm Berman Brain & Spine Institute at LifeBridge Health in Baltimore, Maryland.
What causes migraines?
- Consuming certain foods/beverages/additives (like aged cheeses, alcohol, smoked meats, caffeine, aspartame, MSG)
- Stress
- Certain kinds of light
- Certain smells (like perfumes)
- A change in temperature—up or down—of at least 10 degrees or a barometric pressure change
- Skipping meals or becoming dehydrated
- Hormonal changes (like in women who get migraines just before or during a menstrual cycle)
- An infection
- Getting too little or too much sleep
Some health conditions are also linked to migraines
Many conditions are associated with migraines, including depression, anxiety, fibromyalgia, childhood trauma/abuse, opioid abuse, celiac disease, and irritable bowel syndrome. It’s not clear whether one condition might cause the other—all researchers know is that they are linked (the medical term is “co-morbidity”). In short, if you have one condition, you are more likely to have the other.
People with a history of migraines are also at higher risk of having a stroke or heart attack, so if you get migraines, it’s especially important to keep an eye on your cardiovascular health, eat a healthy diet, and exercise regularly.
What are the signs of a migraine?
A migraine often causes severe, throbbing pain in the head—sometimes on just one side and sometimes on both sides—that lasts anywhere from roughly four to 72 hours. What distinguishes it from other headaches is that the pain is usually accompanied by vomiting or nausea and extreme sensitivity to lights and sounds. This constellation of symptoms can make it hard to function. In other words, if you find yourself having to leave work early or bail on a fun happy hour that you’d been looking forward to, you’re probably dealing with a migraine.
Migraine vs. headache
Many people don’t realize their intense headaches are actually migraines. In fact, recent research shows 90 percent of self-diagnosed sinus headaches are actually migraines. Here’s how the different types of headaches typically strike.
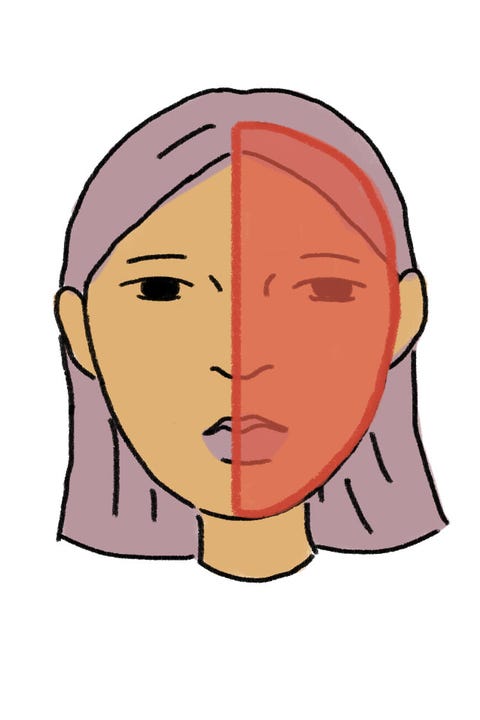
Pain (often only on one side), nausea, vomiting, and hearing or vision disturbances
Mild to moderate pain that feels like a tight band around your head. (This is the most common type of headache.)
Pressure around your cheeks, eyes, and forehead. (Many people who think they’re having a sinus headache are actually experiencing a migraine or tension headache.)

Intense pain on one side of the head, in or around one eye.
The phases of a migraine
There are two phases that may come before a migraine headache, and one that may come after. You may not experience all of these phases each time you have a migraine:
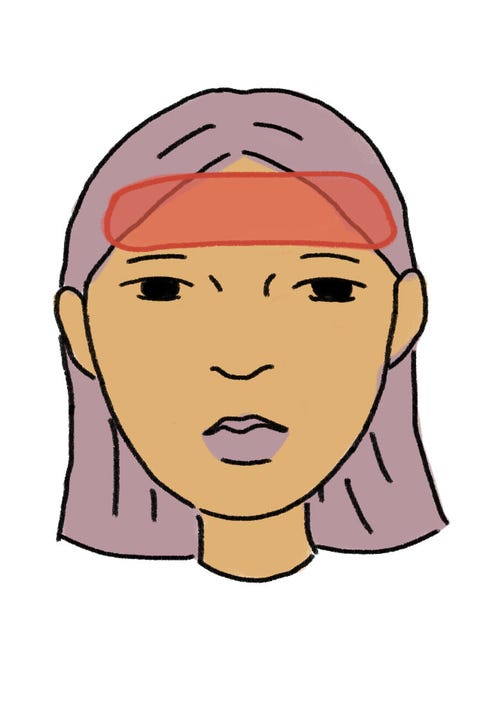
Prodrome
This can hit up to 24 hours before the headache stars. It can include thirstiness, frequent yawning, food cravings, mood changes, or constipation.
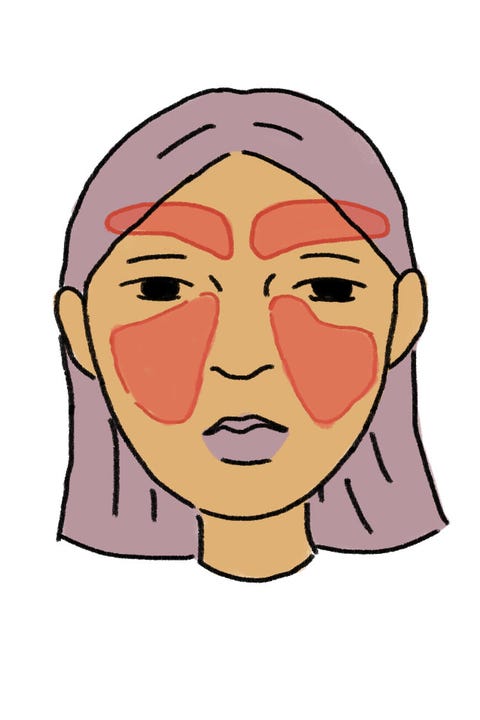
Aura
Post-drome
After the headache dissipates, some people feel drained, confused, or dizzy (kind of like a hangover).
What are the types of migraines?
Up until this point, we’ve focused on classic migraines, but about 20 percent of people who struggle with migraines experience one of these more unusual types. Understanding the type of migraines you’ve been having can help your doctor treat you more effectively, and also give you greater insight into your migraine triggers (so you can be sure to avoid them).
Ocular (or retinal) migraine
You’ll experience roughly 30 minutes of visual disturbances (think: flashes of light, wavy lines, blind spots) in one eye.
Hemiplegic migraine
Expect temporary motor weakness (like one-sided, whole-body paralysis), though this is more common in infants and children.
Migraine with brainstem aura (formerly called basilar migraine)
Signs can include slurred speech, ringing in the ears, gait imbalance, vertigo, double vision, and a lower level of consciousness.
Menstrual migraine
This is a migraine that occurs in a woman either just before or during her menstrual cycle.
Abdominal migraine
Most common in children and adolescents, abdominal migraines usually result in severe nausea/vomiting and possible abdominal pain.
Vestibular migraine
You’ll notice extreme sensitivity to motion and dizziness.
If you’ve ever had a migraine, then you probably understand why preventing them from happening in the first place is just as important as stopping symptoms after they’ve already started. That’s why migraine treatment generally falls into two categories: preventive (stopping headaches before they start) and acute/abortive (stopping headaches as soon as they occur). Each type of treatment is critical in different ways.
PREVENTIVE
Lifestyle changes
Many patients begin by making lifestyle changes, since those are free and don’t require a doctor’s prescription. These lifestyle changes fall into the realm of “basic things your parents always told you to do” like get enough sleep, manage your stress, don’t skip meals, and stay hydrated. They may sound obvious, but with a busy schedule, they’re often easier said than done.
Medications
A primary care physician or neurologist can prescribe a preventative medication to help ward off migraines. In fact, the FDA approved a groundbreaking new drug called erenumab (Aimovig) in May 2018, so patients have more options than ever.
Other non-drug remedies
There are also non-pharmacologic options such as physical therapy, massage, acupuncture, seeing a chiropractor, Botox injections, tinted glasses, biofeedback, or wearing a headband-like device that uses electrodes (this is called transcutaneous supraorbital nerve stimulation or t-SNS).
Nutritional supplements
Your doctor may discuss taking certain nutritional supplements such as magnesium, coq10, or vitamin B2 or B12. Butterbur is another herb that can be used, but recently there have been some concerns about its safety.
ACUTE/ABORTIVE
Over-the-counter medications
Some are basic pain relievers (like aspirin, ibuprofen, naproxen, and acetaminophen) and others are combos (Excedrin Migraine, for instance, is a mix of acetaminophen, aspirin, and caffeine, and Alka Seltzer is a mix of aspirin and two antacids). Pro tip: Any pills that come in a liquid-gel form work faster, which is beneficial when treating a migraine.
Prescription drugs
A primary care physician or neurologist can prescribe various drugs that can help in the moment.
Isolating and hydrating
Retreating to a dark, quiet room, drinking water, and then trying to sleep.
When should I call a doctor about my migraines?
If you’re not getting adequate relief from over-the-counter medications and lifestyle changes, or if you’re taking over-the-counter medications more than 10 to 15 times per month, talk to your primary care physician about your headaches. She will either treat you or refer you to a specialist, such as a neurologist. Taking over-the-counter medications too frequently can sometimes lead to serious side effects (like liver problems) and/or actually make you get headaches more often.
It’s helpful to keep a diary if you experience migraines because you may discover your triggers, which can inform which type of treatment is best for you. Write down what time your migraines occur, how long they last, how you slept the night before, what you ate/drank that day and when, how you felt emotionally that day, etc. Then bring that information to your doctor.
Don’t assume that migraine pain is something you have to live with—there are many treatment options that may help you find significant relief.






















